February 6, 2024
Have you ever had that feeling when you just know that something good or bad is about to happen? That intuitive hunch of someone or something whispering in your ear….”hold on, it’s going to get bumpy” or “hold on, it’s about to get exciting.” I’d venture to say that we’ve all had these intuitive hits at one time or another. It’s a reality of the human experience.
I’ve had a couple of experiences like this in my life, a premonition where I just knew the outcome of an event that was just about to happen. The first time that I can remember this feeling was when I was quite young. There was a carnival hosted by our town’s Lions Club and my siblings and I were each given a couple of dollar’s worth of tickets that we could spend on whatever games of chance the carnival had to offer. Knowing how much a dollar meant, I walked the floor searching for where to place my bets, tickets clutched tightly in my hand. I felt drawn to the roulette wheel and stood to watch how this game of luck and chance was played. Feeling like I understood the rules, I traded two of my tickets for a red paddle with a white number painted on both sides. I wish I could remember the number on that paddle but the surety escapes me. After the roulette wheel was spun, I had the experience of standing outside of myself. I watched as the roulette wheel spun around and around and I just knew that it would stop on my number. I felt knowing in a place that was calm, confident and very sure, as if it had already happened. This place had no time or space or age and yet if felt very much like me.
The wheel landed on my paddle number and I had a choice of prizes. I picked a large beautiful plastic appaloosa horse. He (I knew it was a he) was prancing and majestic and I loved this horse for years, even though at some point his front leg broke and his shiny coating became scratched and faded. The adventures we would go on in my mind were wondrous and he became more than a toy, he was my friend who accompanied me on imaginary rides through far off lands, my friendly reminder that there is a place where knowingness resides and chance deems you worthy of taking a chance. My friend was eventually replaced by vinyl records, hair brushes, bobby pins and a diary, relegated to the toy box for future grandkids to enjoy. Eventually, I heard that he was discarded, his broken leg deemed a potential safety hazard.
The second time I remember this kind of experience happening I was again at a Lion’s Club event while visiting my parents as an adult and I won a chocolate cake. This time it was like “Hey! Remember me?” Again, I just knew my number would be called. Chance had once again appeared in my life and I was reacquainted with that profound sense of knowingness. I need to add that there have been other experiences mainly related to others or in conjunction with others. I think that most of us have had those moments when we thought about someone and then they called or we knew who was on the phone before we answered (obviously pre caller ID because we’re talking synchronicities here). When it came to my twenty-six years as a massage therapist and healer, I could often pick up on the energies surrounding someone else but these experiences were different, very different. They didn’t have the ‘this is for YOU, Peggy’ message engraved on a bright orange sticky note calmly existing in a space of serene certainty.
I’ve shared before that when I received my cancer diagnosis it felt like a cosmic sledgehammer had just sucker punched me from out of left field without any heads up. My knowingness seemed to have failed me, leaving me in the dark without an emotional roadmap. I truly believed that something as serious as stage four cancer could never sneak up on me. I had been doing my work of healing the deep dark places inside for many years and believed that I had an affinity for knowing the unknown.
Without a road map and emotionally devastated, I had to rely on the people chance placed in my path. I began learning how to trust someone else’s knowingness which freed me up to begin looking at deeply buried fears and committing to living life (no matter how much I had left) on my terms. It can be terrifying when uncovering those fears. The worst part is just before the dirt comes off, right before light illuminates the totality of what’s been buried. I find it amazing that the fear of what has been buried is often much worse than the reality. I began by looking death in the face and asking ‘who are you and why am I afraid of you?’ For that matter, ‘who am I?’ My motto has been ‘I don’t want to leave before I’ve completed what I came here to complete.’ My prayer and what I know will happen is that I will know when that time has come… it’s just not today and probably not tomorrow or the next day because after twenty-eight days on treatment line number eight, we know that it’s working.
Last week I had another brain MRI for radiation treatment planning. I also had the mold for my thermoplastic radiation mask done along with the CT simulation scan for SRS (stereotactic radiation surgery) which was to take place in 10-14 days. The trifecta was a follow-up Chest/Abdomen/Pelvis CT scan. The next day a call came in from one of the radiation oncology docs and within that split second before I answered my phone my old friend knowingness made a reappearance: “I’m baaack!” I knew Dr. Nasr would be sharing that after reviewing my scans, the consensus of my oncology team was to wait on SRS as the new treatment was working extremely well on the brain metastasis and the stable areas in my body remained stable to a bit better.
Hello my old friend…and welcome.
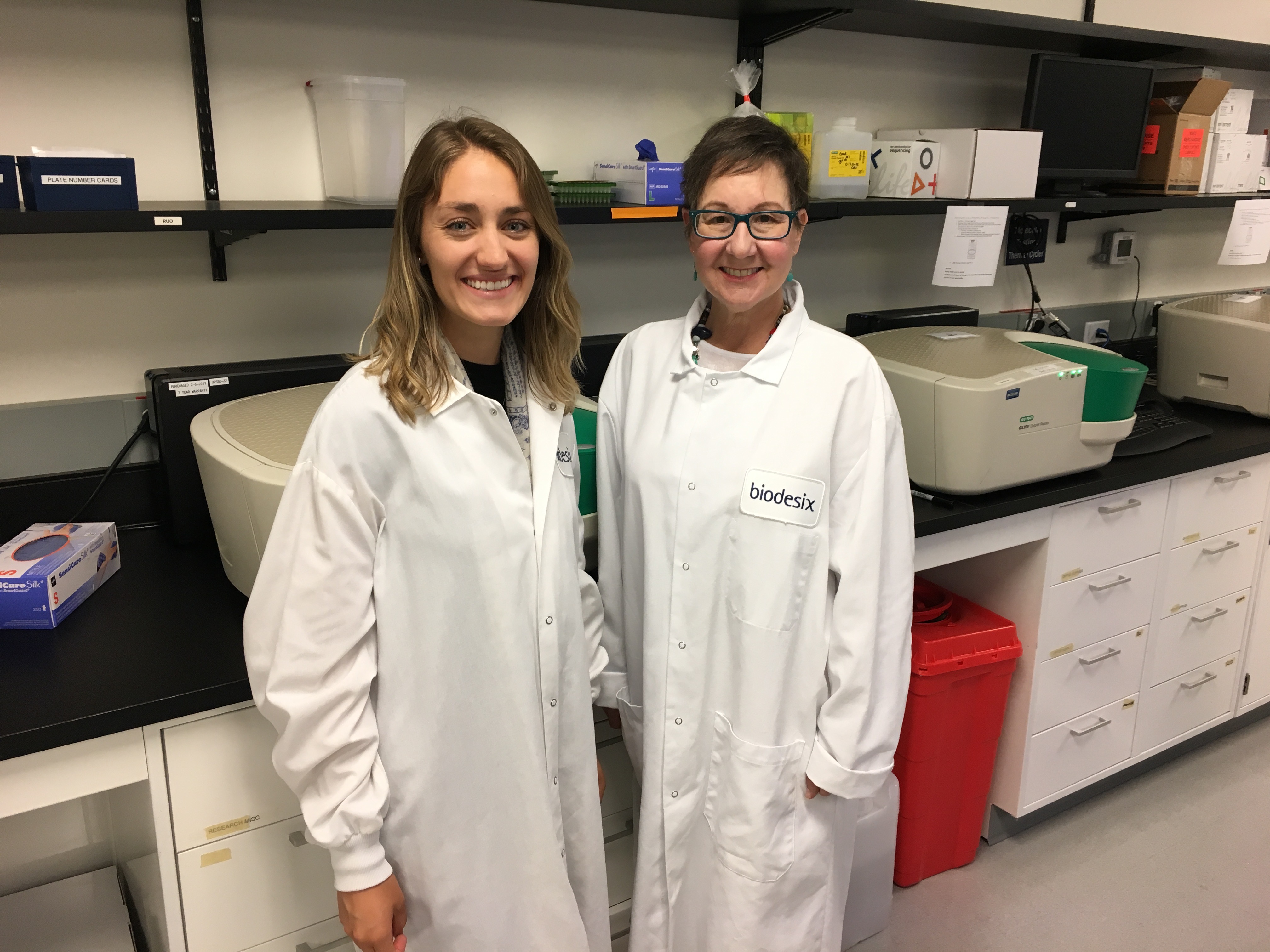
I had an appointment with Dr. Patil this morning and the smile on his face was priceless when he walked into the room. He’s not only a gem of a human being, he’s brilliant and compassionate and a maverick in his chosen field. What I recognize in him that resonates with me is his willingness and ability to act using the knowledge he has and the inspiration he receives … and his being a musician which is the icing on the cake in my book. He was the one who suggested that taking a chance on Mobocertinib was worth pursuing once Enhertu failed. Mobo worked for nineteen months, a good run when it comes to advanced lung cancer. He also was the one to suggest that Tagrisso might be worth a shot and made the necessary calls. Both times he looked at me and said, “I don’t know if this will work but there’s a chance that you could get a good response.” Then he waited to hear my decision for I get final say. Trust is imperative in a doctor patient relationship and he’s well aware of what I’ve experienced the past seven years and seven months. There is also honesty on both our parts as well as respect for the knowns and unknowns of this disease. I asked to see the MRI and CT images and the differences after twenty-eight days was nothing short of incredible. We will scan again in three months.
Knowingness takes many roads as it makes its way to our conscious awareness. Taking chances requires a change in course, red pill-blue pill, choosing which road less traveled we will take into the unknown. Choices walk hand in hand with chances. As I shared, I truly believe that I will know when it’s my time. It might be within a split second or it might be, ‘I’m not doing this anymore. I’m ready for the next adventure.’
For an adventure it will surely be. I know this.
































 Just like most things in life, we all have our own unique relationship with money and how we spend or save it. I like the metaphor of money as energy. It fluctuates, coming in and going out, an exchange in constant motion monitored by the Universal Bank and Trust of the Cosmos. Jim is a saver and I think he would agree with my 37 year observation that he weighs and measures – in depth – the pros and cons of almost every purchase. Our motivations complement each other but I have been known to be a bit more, shall we say – spontaneous. Let’s take the RV we just drove back to Colorado from California. He’s been researching the best (and affordable) makes and models for a solid year. He’s read blogs, looked at hundreds of pictures, made phone calls, went on test drives and we even drove to Nebraska one Saturday to check a couple out. Same make and model, same owner even, just not quite right….and so we waited. Why an RV? Because we want to see and experience this country from a tiny-house-on-wheels perspective and we want to be able to take Tess the wonder dog with us. It is currently unknown if ‘wonder dog’ will remain ‘wonderFUL dog’ when it comes to this type of travel. After everything she’s been through, we know she has the ability to adapt but we also know she has a propensity for motion sickness which will add a certain degree of watchfulness and a supply of Dramamine.
Just like most things in life, we all have our own unique relationship with money and how we spend or save it. I like the metaphor of money as energy. It fluctuates, coming in and going out, an exchange in constant motion monitored by the Universal Bank and Trust of the Cosmos. Jim is a saver and I think he would agree with my 37 year observation that he weighs and measures – in depth – the pros and cons of almost every purchase. Our motivations complement each other but I have been known to be a bit more, shall we say – spontaneous. Let’s take the RV we just drove back to Colorado from California. He’s been researching the best (and affordable) makes and models for a solid year. He’s read blogs, looked at hundreds of pictures, made phone calls, went on test drives and we even drove to Nebraska one Saturday to check a couple out. Same make and model, same owner even, just not quite right….and so we waited. Why an RV? Because we want to see and experience this country from a tiny-house-on-wheels perspective and we want to be able to take Tess the wonder dog with us. It is currently unknown if ‘wonder dog’ will remain ‘wonderFUL dog’ when it comes to this type of travel. After everything she’s been through, we know she has the ability to adapt but we also know she has a propensity for motion sickness which will add a certain degree of watchfulness and a supply of Dramamine.




 After lunch, I spent time with the
After lunch, I spent time with the